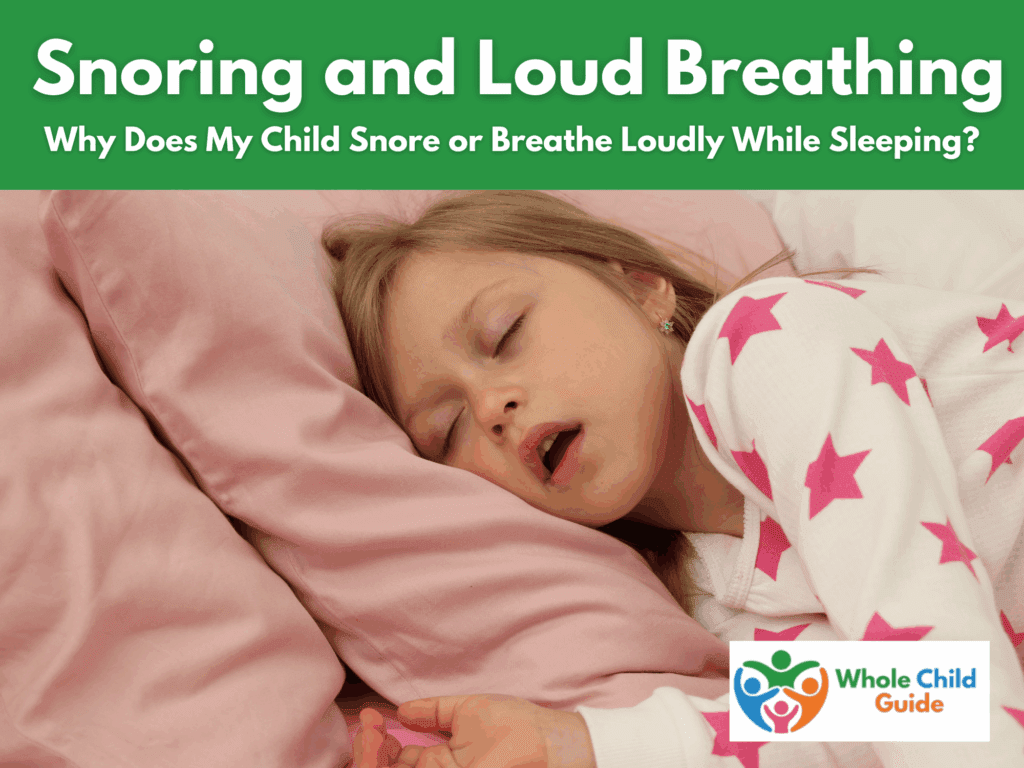
If you’ve ever peeked in on your sleeping child and noticed loud breathing, snoring, or open-mouth sleep, you may have wondered: “Is this normal?” Wondering about a child snoring is common among parents.
Occasional snoring can happen when a child has a cold or allergies, but if your child snores at night regularly, even when they aren’t sick, it may be a sign of something deeper. In fact, persistent pediatric sleep-disordered breathing can impact everything from attention and mood to growth, learning, and emotional regulation.
The good news? When we look at sleep and breathing through a whole child lens, we can uncover the root causes, and help your child (and your whole family) sleep and function better.
What Causes Snoring and Loud Breathing in Children?
There are many possible reasons why your child may breathe loudly or snore during sleep:
- Nasal congestion from allergies, colds, or enlarged adenoids
- Enlarged tonsils, which can partially block airflow
- Deviated septum or chronic sinus issues
- Low oral-motor tone or mouth posture differences
- Mouth breathing related to sensory or muscle tone challenges
- Sleep-disordered breathing such as obstructive sleep apnea
Sometimes, what sounds like “just snoring” can signal disrupted airflow that prevents deep, restorative sleep. This can lead to frequent night wakings, restless movement, and daytime fatigue. You may see this in toddlers who wake frequently at night.
If you notice loud breathing during sleep in kids, consistent mouth breathing, or pauses in breathing, it’s important to explore what’s behind it.
The Whole Child Impact of Sleep-Disordered Breathing
Sleep and breathing are whole-body processes. When a child doesn’t breathe efficiently during sleep, the effects ripple across physical, emotional, and developmental domains:
- Daytime behavior: irritability, hyperactivity, or inattention (often mistaken for ADHD).
- Learning and memory: difficulty focusing or retaining new information.
- Mood regulation: increased anxiety, frustration, or emotional swings.
- Growth and development: oxygen levels affect metabolism and hormone regulation.
- Speech and feeding: oral-motor differences that impact articulation or swallowing can also influence nighttime breathing patterns.
This is why whole child sleep support means addressing breathing, motor skills, sensory regulation, and emotional well-being together.
How Mouth Breathing Affects Development
Here at Whole Child Guide, we take a whole child perspective, and that means considering aspects that impact child development that might not be considered right away. Mouth breathing and child development are closely connected. When kids habitually breathe through their mouths instead of their noses, it can affect:
- Jaw and facial growth (narrow palate, dental crowding)
- Oral posture and tongue position
- Speech sound production
- Feeding and swallowing mechanics
- Sleep quality and oxygen intake
Speech therapists (SLPs) and orofacial myologists can assess mouth and tongue posture, helping retrain breathing and oral-motor patterns that support healthy airway function.
Learn more about speech therapy’s developmental role in How Can Speech Therapy Near Me Help?.
How Occupational and Physical Therapists Can Help
An occupational therapist (OT) looks at how sensory processing affects relaxation and body positioning during sleep. They may help with:
- Sensory-friendly sleep environments
- Body awareness and calming routines
- Postural supports that promote safe, comfortable breathing
Read more about how OTs address sleep in My Child Has Sensory Issues . What Can We Do to Help Them Fall Asleep and Stay Asleep?.
Physical therapists (PTs) address motor tone, neck and shoulder alignment, and breathing mechanics that influence airway support.
Learn more about PT’s role in growth and comfort in How Can Physical Therapy Near Me Help?.
When to Consult a Doctor or Specialist
If your child snores but isn’t sick, talk to your pediatrician about next steps. They may refer you to:
- An ear, nose, and throat (ENT) specialist to evaluate tonsils, adenoids, or nasal structure.
- A pediatric sleep specialist to conduct a sleep study for pediatric sleep-disordered breathing.
- A dentist or orthodontist trained in airway development.
In some cases, medical interventions, like allergy management, tonsil removal, or oral appliance therapy, can make a dramatic difference.
Supporting Better Sleep While You Wait
While you explore medical and therapeutic options, these simple adjustments can improve nighttime comfort:
- Elevate your child’s head slightly for easier airflow.
- Keep the bedroom cool and use a humidifier if the air is dry.
- Encourage daytime nose breathing with gentle reminders and play-based exercises.
- Maintain consistent sleep routines and sensory-calming activities. (See gentle sleep ideas here.)
- Reduce congestion triggers. Avoid smoke exposure and manage allergies.
These steps help create a whole child sleep support system that blends environment, movement, and calm routines.
Whole Child Collaboration for Healthy Sleep
When professionals collaborate, children thrive. Supporting breathing during sleep often involves a team:
- ENT or pediatrician – identifies medical or structural causes.
- Speech therapist or myofunctional therapist – improves oral-motor tone and breathing habits.
- Occupational therapist – regulates sensory and environmental comfort.
- Physical therapist – optimizes posture and alignment for clear airflow.
- Parent coach or sleep consultant – helps build consistent bedtime routines and reduce anxiety.
You can connect with these professionals through the Whole Child Guide Directory… your starting point for finding coordinated, family-centered care.
When to Seek Immediate Help
If your child snores loudly every night, gasps, pauses in breathing, or seems excessively tired during the day, contact your pediatrician right away. These could be signs of obstructive sleep apnea, which requires medical evaluation.
The Bottom Line
Snoring isn’t always just snoring. It’s a window into how your child’s body, brain, and environment are working together. When we address sleep and breathing from a whole child perspective, with medical insight and developmental expertise we give kids the foundation they need to grow, learn, and thrive.